February 15, 2018
Stanton A. Glantz, PhD
The FDA should not adopt the nicotine “harm reduction” paradigm because doing so is likely to increase the amount of smoking-caused disease and death
My colleagues and I have submitted this public comment to FDA in response to its request for information about its comprehensive nicotine policy and alternative forms of nicotine delivery. The tracking number is 1k2-91ii-k7sy . A PDF of the comment is here.
The FDA should not adopt the nicotine “harm reduction” paradigm because doing so is likely to increase the amount of smoking-caused disease and death
Docket No. FDA-2017-N-6529
Dorie Apollonio, PhD, Stanton A. Glantz, PhD, Sharon Hall, PhD, Lauren Lempert, JD, MPH, Gideon St.Helen, PhD, and Janice Tsoh, PhD
University of California, San Francisco
February 15, 2018
The goal of FDA’s approach to evaluating nicotine replacement therapies should be complete cessation, not “harm reduction,” because the likely result of adopting the tobacco industry’s harm reduction frame[1],[2] will be continued smoking and increases in overall harm. In addition, to ensure that it is effective, FDA should emphasize that use of NRT must be accompanied by effective counseling and cessation support, and should discourage dual use with other tobacco products.
The essential starting point for FDA’s consideration of the public health, scientific, regulatory, and legal considerations relating to nicotine replacement therapy (NRT) products and their use in tobacco cessation must be the current scientific evidence showing no level of combustible tobacco use is safe. For example, smoking one cigarette a day is sufficient to significantly increase the risks for developing stroke and coronary heart disease.[3]
Smoking reduction should not be the goal or an acceptable outcome of any NRT treatment regimen. Rather, complete cigarette cessation and complete abstinence from any alternative tobacco products should continue to be the desired endpoint.
Scientific evidence shows that NRT used without counselling is ineffective, or even harmful, in terms of promoting cessation.[4] The tobacco companies have long understood this fact and are now entering the over-the-counter (OTC) NRT business (without providing the needed counselling) as part of their plans to hold on to customers who might otherwise stop smoking entirely.[5]
Given FDA’s mission to protect and promote public health, the most effective and least harmful way to provide NRT is to restrict their use to smokers whose quit attempts are medically supervised. NRT labeling should include warnings about the potential harms of improperly using NRT together with other forms of tobacco products and the risks of using unsupervised NRT without monitoring by a health professional or smoking cessation counseling program with the end-goal of achieving smoking cessation.
Any efforts to improve OTC NRT effectiveness should include direct efforts to improve adherence to NRT, including, but not limited to, public education, making NRT use instructions easy to understand for consumers with limited health literacy, and integrating smoking cessation counseling support with OTC NRT use.
We elaborate on these points below and respond to specific questions FDA posed in its Request for Comments.
1.Might there be ways to improve upon the currently available delivery systems to yield new OTC NRT products that might be more effective? If so, what evidence would be needed to support such changes, and how should they be evaluated?
Any new OTC NRT product must be evaluated for its abuse liability and potential, specifically within the context of how the product(s) may be consumed by users, including whether such new products may result in the increased likelihood of concurrent use of cigarettes and/or other tobacco products both in the short and long term. Complete cigarette cessation and complete abstinence from any alternative tobacco products should be the desired endpoint, rather than reduction in consumption of cigarettes and/or other tobacco products given that there is little evidence to support health benefits or reduction of harm by continued tobacco use at any level.[6],[7] The FDA needs to be particularly cognizant of the evidence, discussed above, that NRT use without smoking cessation counseling or support reduces the likelihood of successful smoking cessation, so increases, rather than reduces, harm.
While adherence to NRT is a consistent predictor of smoking cessation,[8],[9] many smokers do not use NRT correctly and/or discontinue NRT early.[10] Smokers from vulnerable groups where smoking prevalence remains high, such as those who are socio-economically disadvantaged and those with psychiatric comorbidities, are reportedly more likely to be non-adherent to NRT.[11],[12] Qualitative research suggests several factors associated with NRT non-adherence, including limited health literacy, misunderstanding the purpose of NRT and its correct usage, and experience with and fear of side effects.[13],[14]
Non-adherence to NRT can contribute to the limited effectiveness or counter-productive effects of NRT observed in real-world settings. Specifically, evidence shows that NRT used without counselling is ineffective or even harmful in terms of promoting cessation.[15]
Thus, FDA should direct efforts to improve consumers’ adherence to NRT as part of the crucial effort devoted to improve OTC NRT effectiveness. Efforts to increase NRT adherence should include, but not be limited to: (1) public education via multiple channels to reach all population groups, and specifically those with high smoking prevalence; (2) making NRT use instructions easy to understand for consumers with limited health literacy; and (3) integrating smoking cessation counseling support with OTC NRT use.
If these efforts fail, FDA should remove NRT from OTC sale and put it back as a prescription drug in an effort to see that its use is properly supervised and monitored.
2.Are there additional indications or regimens for OTC NRT products that could be explored? Concepts to consider could include relapse prevention, craving reduction, maintenance, reduce to quit, use of short- and long-acting products in combination, or cessation of non-cigarette tobacco products. What evidence would be needed to support each indication or regimen?
For the reasons discussed throughout the rest of this comment, using OTC NRT without evidence-based smoking cessation support and without an endpoint as complete abstinence from any form of tobacco products, is unlikely to produce health benefits and should not be recommended.
3.What data would be required to demonstrate health benefits of reduction in consumption of combustible tobacco products?
Foremost, no level of combustible tobacco use is safe, and reduction should not be the goal or an acceptable outcome of any treatment regimen.
The risk of cardiovascular diseases, which kill more smokers than cancer or respiratory diseases combined each year,[16] is almost as high among low consumption or infrequent smokers compared to high consumption smokers. In 2012, an estimated 85.6 million U.S. adults (35%) had at least one cardiovascular disease[17] and in 2013, cardiovascular diseases accounted for roughly 1 in 3 (30.8%) U.S. deaths (800,937 of 2,596,993 deaths).[18] Of the five major risk factors for cardiovascular diseases (hypertension, smoking, poor diet, insufficient physical activity, and abnormal glucose levels) smoking is the second in terms of contribution to cardiovascular disease incidence in the U.S.[19] Given the steep dose-response relationship between smoking and cardiovascular disease risk, the high prevalence of cardiovascular diseases in the U.S., and the fact that most smokers actually die from cardiovascular diseases and not from cancer or respiratory diseases, FDA should not encourage reduction as a goal or acceptable outcome of a treatment regimen.
In theory there may be some reduction in risk of some other disease outcomes for individuals who significantly reduce their smoking consumption. However, because to date there has been no scientific evidence supporting this theory, both short and long-term rigorous studies will be required to demonstrate potential benefits of reduction before the FDA advocates this as a public health strategy.
Short-term studies can compare biomarkers of exposure and effect during regular consumption and reduced consumption. The most robust study design would be within-subject comparisons, such as crossover studies, or randomized controlled trials. The studies should be of sufficient duration to allow characterization of biomarkers of longer term tobacco smoke exposure and not just recent use (as in a few days). An appropriate biomarker of exposure is the tobacco-specific nitrosamine, NNAL. NNAL is a biomarker of exposure to NNK, both of which are potent pulmonary carcinogens.[20] NNAL has a half-life of about 2 weeks and would be ideal to assess smoking patterns over several weeks to months. Reduction in NNAL would indicate reduction in exposure to tobacco smoke (and not just reduction in number of cigarettes smoked since people can smoke fewer cigarettes but compensate by smoking each cigarette more intensely). Short-term studies should also characterize changes in biomarkers of pathophysiological mechanisms that are associated with increased risk of diseases. Oxidative stress, for example, underlies many diseases, including cardiopulmonary diseases and cancer. Thus, biomarkers of oxidative stress should be measured. Other endpoints include markers of respiratory injury, DNA adducts (to assess cancer risk), and intermediate physiological outcomes that may indicate increased disease risk such as heart rate and blood pressure changes, lung function, and measures of endothelial function, such as flow mediated dilation (FMD). Favorable changes in biomarkers of exposure to tobacco smoke and various biomarkers of effect would indicate reduced risk of diseases from reduction.
Long-term studies can include observational studies to examine risk of tobacco-related diseases among smokers who reduce consumption and those who do not. These studies would require large sample sizes. Longitudinal cohort studies would be ideal but these studies are expensive and given the latency between tobacco use and clinical endpoints, they would be more difficult to carry. Case-control studies, although retrospective, would be more practical. Cross-sectional studies to assess prevalence of diseases, symptoms, levels of biomarkers of effects and exposure among people who reduce consumption and those who do not can also provide useful information on potential benefits of reduction. However, cross-sectional studies are limited in that they do not include a temporal component.
In summary, it is unlikely that smoking reduction would result in decreased cardiovascular disease risk, the disease that kills most smokers. For that reason, reduction should not be a goal in smoking treatment.
4.Are there OTC NRT products that could be studied for use in combination that might result in reduced tobacco-related health impacts? What evidence would be needed to support the safety and efficacy of these products when used in combination?
Before considering which NRT products could be used in combination and how they should be used to increase safety and efficacy, FDA must first consider whether using OTC NRT products in combination may result in an increased likelihood of dual or concurrent use of various tobacco products, and the potential tobacco-related health impacts resulting from such use. Emerging scientific evidence shows significant increased health risks associated with dual use of tobacco products, and a recent analysis of population-based data showed that current adult cigarette smokers in the U.S. who report using e-cigarettes had greater disease symptoms such as chest pains, ulcers or sores in the month, cold or wheezing.[21] Thus, the potential increased harm that may result from a combination of nicotine/tobacco products use should be given serious consideration.
A meta-analysis of all available studies (published through February 14, 2018) examining the relationship between e-cigarette use and smoking cessation shows that, in the real world, for most smokers’ e-cigarette use substantially reduces the odds of smoking cessation.[22]
FDA’s proposal to use so-called “innovative technologies” such as e-cigarettes or heated tobacco products is therefore not a good strategy to tackle nicotine regulation or addiction because of its likelihood to increase dual or concurrent use of tobacco products, including cigarettes, cigars, and hookah, and its likelihood to attract youth and adolescents to initiate tobacco use.
5.Is there other information that could be added to labeling for currently approved or new dosage forms of OTC NRT products that would maximize their ability to be used to support smoking cessation? Please consider the various sections of the Drug Facts labeling, including the Uses, Warnings, and Directions sections.
It is important to note that while NRT is a proven cessation intervention when combined with counselling, the evidence consistently shows that NRT used without counselling is ineffective – or even harmful – in terms of promoting cessation.[23] Many states and medical systems provide NRT alone; this practice should be discouraged as a wasteful – and possibly counterproductive – use of resources. OTC NRT labeling should clearly direct NRT users to obtain smoking cessation support from health professionals and/or a smoking cessation counseling program because unsupported OTC NRT may make it harder to quit. Additionally, labeling should include warnings about the potential harms of improperly using NRT together with other forms of tobacco products unless directed or monitored by a health professional or a smoking cessation counseling program with the end-goal of achieving smoking cessation.
This issue is of particular concern because the tobacco industry is now entering the NRT business as part of a plan to retain customers, informed by their understanding that NRT use without counselling likely depresses cessation.
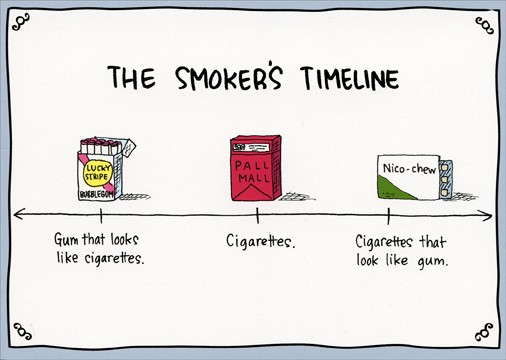
The following cartoon illustration, “The Smoker’s Timeline” depicts the danger of encouraging NRT use without provision of cessation counseling support.
As Apollonio and Glantz[24] noted:
Major tobacco companies in the United States and the United Kingdom viewed NRT, even when it was only available by prescription, as a recreational product that could maintain and possibly expand the use of nicotine as smoking became less socially acceptable. Although NRT was approved for cessation, tobacco industry research found in the early 1990s that many smokers used it in combination with cigarettes and that smokers who used NRT for cessation would otherwise have quit outright. 49–51,53,54
In the 21st century, medical research began to find similar results. The majority of smokers who receive prescription NRT receive counseling on how to use the medication.59 Initial clinical trials suggesting comparable effectiveness for OTC NRT relied on simulated OTC use rather than real-world OTC use.11–16 Follow-up population studies of OTC NRT showed it did not improve—and could impede—cessation, without an organized cessation program.8,9,17,18 Outside of monitored settings, NRT is often used for shorter periods than recommended and not combined with behavioral counseling.10 These findings are consistent even among individuals motivated to quit: a follow-up study of participants enrolled in a clinical trial of nicotine patch users found that after 8 years, there was no statistically significant difference in abstinence for patch users than nonusers.60 Moreover, smokers who used over-the-counter NRT were significantly less likely to quit than were smokers who did not use any cessation aids.8,9
Tobacco companies expressed interest in developing and marketing alternative products containing nicotine as early as the 1950s, but they were concerned about marketing them because doing so could lead to FDA regulation. In 2009, following new FDA regulation of cigarettes, tobacco companies began selling the alternative nicotine products they had first proposed decades earlier.61 In 2014, RJ Reynolds Tobacco began selling its nicotine gum, Zonnic, throughout the United States. Internally, RJR classified Zonnic with its e-cigarette brand Vuse, considering both products to be part of its “quest toward becoming a ‘total tobacco company.’”4 Reflecting this ambition, marketing in 2015 for Zonnic suggested that smokers could use it with cigarettes: “Quitting doesn’t have to feel like all or nothing.”61 This marketing is consistent with tobacco industry research that found many smokers used NRT in combination with cigarettes instead of as a means to quit smoking. Philip Morris began marketing nicotine lozenges in 2016.5,6
…
Tobacco industry research from the 1970s forward treated all products containing nicotine—including cigarettes, e-cigarettes and their precursors, and others (e.g., gums, patches, and candy)—as part of a single market: the nicotine delivery, or Craving Relief market. Industry marketing anticipates that noncigarette nicotine delivery products will be used by smokers for whom smoking is unacceptable, thus facilitating and normalizing lifelong nicotine addiction. These findings suggest that the least harmful way to sell nicotine delivery products is to restrict them to smokers whose quit attempts are medically supervised, consistent with the original studies of NRT for smoking cessation.7
[Citations in this excerpt are found in: Apollonio D, Glantz SA. Tobacco Industry Research on Nicotine Replacement Therapy: "If Anyone Is Going to Take Away Our Business It Should Be Us". Am J Public Health. 2017 Oct;107(10):1636-1642. doi: 10.2105/AJPH.2017.303935. Epub 2017 Aug 17.]
These findings provide further evidence that FDA should not support the tobacco industry’s playbook by including e-cigarettes and other supposedly “innovative technologies” as part of its nicotine reduction strategy. Indeed, such a strategy is more likely to facilitate or normalize addiction to nicotine, especially among youth, rather than reduce nicotine addiction.
In conclusion, the following information should be clearly provided in the Uses, Directions, and Warnings sections of the Drug Facts labeling on any OTC NRT products:
-
Uses:
The use of these products should be limited to smoking cessation. While smoking cessation for some individuals may involve gradual reduction of cigarettes/tobacco product consumption, the ultimate goal of using these products should be directed toward complete smoking abstinence.
-
Directions:
The use of NRT should be integrated with concurrent use/participation in a smoking cessation program* to increase likelihood of achieving smoking abstinence.
In addition, the combined use of faster-acting NRT medications with nicotine patch, or use of NRT prior to quit date or for smoking reduction should be guided by a health professional or a smoking cessation program as part of a quit attempt with an endpoint as achieving complete smoking abstinence from cigarettes and/or other forms of tobacco products.
-
Warnings:
Use of NRT products without smoking cessation counseling support or consultation with a health provider may decrease the likelihood of quitting smoking.
* Examples of evidence-based accessable free resources of smoking cessation programs include the Quitline and smokefree.gov resources, advice from healthcare providers, smoking cessation classes that use evidence-based curriculum from trusted authority such as the American Lung Association, American Heart Association, American Cancer Society, and the National Institutes of Health / National Cancer Institute.
6.Generally, the labeling of OTC NRT products contains a dosing schedule based on duration of use, and FDA has recommended the labeling on OTC NRT products be modified to include the following: “If you feel you need to use [the NRT product] for a longer period to keep from smoking, talk to your health care provider.” What is the impact of longer term NRT treatment? What is the impact on likelihood of cessation or relapse prevention? What data would support an affirmative recommendation to use approved OTC NRT products for durations that exceed those currently included in the Drug Facts labeling of approved OTC NRT products, or would support a chronic or maintenance drug treatment indication for such products?
Scientific evidence has not demonstrated extended NRT use (beyond 12 weeks of recommendation) and smoking abstinence.[25] However, extended cognitive behavioral smoking cessation treatments, with or without availability of NRT, have produced unparalleled long-term abstinence rates from 45% to 55% abstinence rates at 1 year or beyond.[26], [27] Mobile interventions may be an ideal medium to provide extended treatments or smoking cessation support. In 2017, the Pew Research Center reported that 95% of Americans own a cellphone[28] and 70% use social media.[29] Given mobile interventions for tobacco use have a broad reach, extended treatment or support can be implemented after an intensive face-to-face intervention, or in a form of electronic contacts with tailored and extensive contents, or to provide support for extended prescription to yield high abstinence rates.[30]
While extended use of NRT has not been linked to safety concerns, it is essential for FDA to inform the public regarding the importance of receiving smoking cessation counseling support with NRT use in order to achieve long-term smoking abstinence. Importantly, the evidence consistently shows that NRT used without counselling is ineffective – or even harmful – in terms of promoting cessation.[31] Any provision of extended NRT treatment should be accompanied by evidence-based smoking cessation support.
In summary, FDA’s approach to NRT must be based on the following evidence-based points:
(1)there is no safe level of combustible tobacco use;
(2)smoking reduction should not be the goal or an acceptable outcome of any NRT treatment regimen;
(3)complete cigarette cessation and complete abstinence from any alternative tobacco products should be the desired endpoint;
(4)NRT used without counselling is ineffective, or even harmful, in terms of promoting cessation;
(5)OTC NRT effectiveness requires direct efforts to improve adherence;
(6)Combined use of NRT, especially with e-cigarettes and other so-called “innovative technologies,” is likely to be associated with dual use with other tobacco products and is more likely to facilitate nicotine addiction, rather than reduce addiction; and
NRT labeling should include clear directions and warnings to direct users to use NRT with smoking cessation support and to use NRT with the end-goal of complete abstinence of any tobacco products.
[1] Peeters S, Gilmore AB. Understanding the emergence of the tobacco industry's use of the term tobacco harm reduction in order to inform public health policy. Tob Control. 2015 Mar;24(2):182-9. doi: 10.1136/tobaccocontrol-2013-051502. Epub 2014 Jan 22.
[2] Peeters S, Gilmore AB. Transnational tobacco company interests in smokeless tobacco in Europe: analysis of internal industry documents and contemporary industry materials. PLoS Med. 2013;10(9):e1001506. doi: 10.1371/journal.pmed.1001506. Epub 2013 Sep 10.
[3] Hackshaw A, Morris JK, Boniface S, Tang JL, Milenkovic D. Low cigarette consumption and risk of coronary heart disease and stroke: meta-analysis of 141 cohort studies in 55 study reports. BMJ. 2018;360:j5855. Epub 2018/01/26. doi: 10.1136/bmj.j5855. PubMed PMID: 29367388.
[4] Kotz D, Brown J, West R. Prospective cohort study of the effectiveness of smoking cessation treatments used in the “real world.” Mayo Clin Proc. 2014;89(10):1360–1367. Kotz D, Brown J, West R. “Real-world” effectiveness of smoking cessation treatments: a population study. Addiction. 2014;109(3):491–499. Leas, EC, et al, Effectiveness of Pharmaceutical Smoking Cessation Aids in a Nationally Representative Cohort of American Smokers. JNCI: Journal of the National Cancer Institute, djx240, https://doi.org/10.1093/jnci/djx240. Published: 21 December 2017.
[5] Apollonio D, Glantz SA. Tobacco Industry Research on Nicotine Replacement Therapy: "If Anyone Is Going to Take Away Our Business It Should Be Us". Am J Public Health. 2017 Oct;107(10):1636-1642. doi: 10.2105/AJPH.2017.303935. Epub 2017 Aug 17.
[6] U.S. Department of Health and Human Services. The Health Consequences of Smoking-50 Years of Progress: A Report of the Surgeon General. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2014.
[7] Lindson-Hawley N, Hartmann-Boyce J, Fanshawe TR, Begh R, Farley A, Lancaster T. Interventions to reduce harm from continued tobacco use. Cochrane Database of Systematic Reviews 2016, Issue 10. Art. No.: CD005231. DOI: 10.1002/14651858.CD005231.pub3.
[8] Okuyemi KS, Goldade K, Whembolua GL, Thomas JL, Eischen S, Guo H, Connett JE, Grant J, Ahluwalia JS, Resnicow K, Owen G, Gelberg L, Jarlais DD. Smoking characteristics and comorbidities in the power to quit randomized clinical trial for homeless smokers. Nicotine Tob Res. 2013 Jan; 15(1):22-8.
[9] Schnoll RA, Hitsman B, Blazekovic S, et al. Longitudinal changes in smoking abstinence symptoms and alternative reinforcers predict long-term smoking cessation outcomes. Drug Alcohol Depend 2016;165:245-52. doi: 10.1016/j.drugalcdep.2016.06.017
[10] Burns EK, Levinson AH. Discontinuation of nicotine replacement therapy among smoking-cessation attempters. Am J Prev Med 2008;34(3):212-5. doi: 10.1016/j.amepre.2007.11.010
[11] Handschin J, Hitsman B, Blazekovic S, Veluz-Wilkins A, Wileyto EP, Leone FT et al. Factors Associated with Adherence to Transdermal Nicotine Patches within a Smoking Cessation Effectiveness Trial. Journal of Smoking Cessation. 2017 Mar 9;1-11. Available from, DOI: 10.1017/jsc.2017.2
[12] Ojo-Fati O, Thomas J, Vogel R, Ogedegbe O, Jean-Louis G, Okuyemi K. Predictors of Adherence to Nicotine Replacement Therapy (Nicotine Patch) Among Homeless Persons Enrolled in a Randomized Controlled Trial Targeting Smoking Cessation. Journal of family medicine. 2016;3(7):1079
[13] Tsang IK, Tsoh JY, Wong C, et al. Understanding and use of nicotine replacement therapy and nonpharmacologic smoking cessation strategies among Chinese and Vietnamese smokers and their families. Prev Chronic Dis 2014;11:E26. doi: 10.5888/pcd11.130299
[14] Burns EK, Levinson AH. Discontinuation of nicotine replacement therapy among smoking-cessation attempters. Am J Prev Med 2008;34(3):212-5. doi: 10.1016/j.amepre.2007.11.010
[15] Kotz D, Brown J, West R. Prospective cohort study of the effectiveness of smoking cessation treatments used in the “real world.” Mayo Clin Proc. 2014;89(10):1360–1367.
Kotz D, Brown J, West R. “Real-world” effectiveness of smoking cessation treatments: a population study. Addiction. 2014;109(3):491–499.
Leas, EC, et al, Effectiveness of Pharmaceutical Smoking Cessation Aids in a Nationally Representative Cohort of American Smokers. JNCI: Journal of the National Cancer Institute, djx240, https://doi.org/10.1093/jnci/djx240. Published: 21 December 2017.
[16] Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2016 update. Circulation. 2016;133(4):e38-e360.
[17] Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2016 update. Circulation. 2016;133(4):e38-e360.
[18] National Center for Health Statistics. Mortality multiple cause micro-data files, 2013: public-use data file and documentation: NHLBI tabulations. 2014.
[19] Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2016 update. Circulation. 2016;133(4):e38-e360.
[20] Hecht SS. Tobacco smoke carcinogens and lung cancer. J Natl Cancer Inst. 1999;91(14):1194-210.
[21] Yao T, Max W, Sung HY, Glantz SA, Goldberg RL, Wang JB, Wang Y, Lightwood J, Cataldo J. Relationship between spending on electronic cigarettes, 30-day use, and disease symptoms among current adult cigarette smokers in the U.S. PLoS ONE. 2017;12(11):e0187399. Epub 2017/11/08. doi: 10.1371/journal.pone.0187399. PubMed PMID: 29112988; PubMed Central PMCID: PMCPMC5675454.
[22] Glantz S, Bareham D. E-Cigarettes: Use, Effects on Smoking, Risks, and Policy Implications. Annual Review of Public Health 2018 39:1 http://www.annualreviews.org/doi/10.1146/annurev-publhealth-040617-013757
[23] Kotz D, Brown J, West R. Prospective cohort study of the effectiveness of smoking cessation treatments used in the “real world.” Mayo Clin Proc. 2014;89(10):1360–1367.
Kotz D, Brown J, West R. “Real-world” effectiveness of smoking cessation treatments: a population study. Addiction. 2014;109(3):491–499.
Leas, EC, et al, Effectiveness of Pharmaceutical Smoking Cessation Aids in a Nationally Representative Cohort of American Smokers. JNCI: Journal of the National Cancer Institute, djx240, https://doi.org/10.1093/jnci/djx240. Published: 21 December 2017.
[24] Apollonio D, Glantz SA. Tobacco Industry Research on Nicotine Replacement Therapy: "If Anyone Is Going to Take Away Our Business It Should Be Us". Am J Public Health. 2017 Oct;107(10):1636-1642. doi: 10.2105/AJPH.2017.303935. Epub 2017 Aug 17.
[25] Stead LF, Perera R, Bullen C, Mant D, Hartmann-Boyce J, Cahill K, Lancaster T. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev. 2012;11:CD000146. Epub 2012/11/16. doi: 10.1002/14651858.CD000146.pub4. PubMed PMID: 23152200.
Mendelsohn C. Optimising nicotine replacement therapy in clinical practice. Aust Fam Physician. 2013;42(5):305-9. Epub 2013/06/20. PubMed PMID: 23781531.
Webb Hooper M, Dietz NA, Wilson JC. Smoking Urges During Treatment and Long-Term Cessation among Low-Income African Americans. Ethn Dis. 2017;27(4):395-402. Epub 2017/12/12. doi: 10.18865/ed.27.4.395. PubMed PMID: 29225440; PubMed Central PMCID: PMCPMC5720949.
[26] Hall SM, Humfleet GL, Munoz RF, Reus VI, Robbins JA, Prochaska JJ. Extended treatment of older cigarette smokers. Addiction. 2009;104(6):1043-52. doi: 10.1111/j.1360-0443.2009.02548.x. PubMed PMID: 19392908; PubMed Central PMCID: PMC2718733.
[27] Hall SM, Humfleet GL, Munoz RF, Reus VI, Prochaska JJ, Robbins JA. Using extended cognitive behavioral treatment and medication to treat dependent smokers. Am J Public Health. 2011;101(12):2349-56. doi: 10.2105/AJPH.2010.300084. PubMed PMID: 21653904; PMCID: PMC3222443.
[28] http://www.pewinternet.org/fact-sheet/mobile/
[29] http://www.pewinternet.org/fact-sheet/social-media/
[30] Hall, S. M. Commentary on Laude, et. al.: Extended treatment of cigarette smoking. Addiction. 2017; 112 (8) 1460-1461. doi: 10.1111/add.13884.
[31] Kotz D, Brown J, West R. Prospective cohort study of the effectiveness of smoking cessation treatments used in the “real world.” Mayo Clin Proc. 2014;89(10):1360–1367. Kotz D, Brown J, West R. “Real-world” effectiveness of smoking cessation treatments: a population study. Addiction. 2014;109(3):491–499. Leas, EC, et al, Effectiveness of Pharmaceutical Smoking Cessation Aids in a Nationally Representative Cohort of American Smokers. JNCI: Journal of the National Cancer Institute, djx240, https://doi.org/10.1093/jnci/djx240. Published: 21 December 2017.

Add new comment