April 9, 2018
Stanton A. Glantz, PhD
While several studies have been published showing some e-cig users quit more, the overall picture remains negative
There have been several studies published recently (the latest is here) showing that daily users of high nicotine delivery e-cigarette systems quit more than people who don’t use e-cigarettes. These studies also show depressed quitting or no effect of non-daily users of high delivery systems as well as cig-alikes. Because only a small minority of e-cigarette users (10-20%) are daily users of high delivery systems, the overall population health effect of e-cigarettes on smoking cessation remains negative, i.e., on average smokers who use e-cigarettes are less likely to quit than smokers who do not use e-cigarettes.
In 2016 Sara Kalkhoran and I published a meta-analysis that considered all the available evidence at the time, which found an overall negative effect of e-cigarette use on smoking cessation. (In that paper we also suggested that there was some evidence that heavy users of high delivery systems quit more; as noted above, the evidence to support this view had grown stronger.)
Since then I have been updating the meta-analysis every time a new study comes out. The conclusion that, overall, e-cigarettes depress quitting has been remarkably stable.
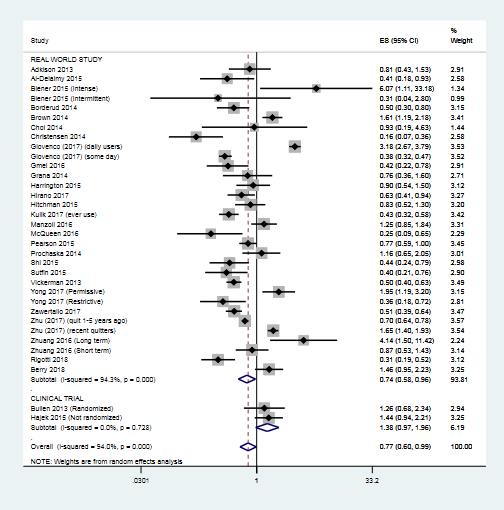
Here is the current meta-analysis of all the papers on the subject of e-cigarettes and quitting that I know about. (If anyone knows of any that I missed, please send them to me and I will add them.) Overall the odds of quitting are significantly reduced (OR 0.77, 95% CI 0.60-0.99) among smokers who use e-cigarettes compared to smokers who do not use e-cigarettes.
This result is essentially the same as Kalkhoran and I found (OR 0.72, 95% CI 0.57-0.91). The stability of this estimate as new data become available is important.
This finding is important as the FDA thinks about its “comprehensive nicotine policy,” which seems to be premised on the idea that smokers should be pushed from combusted cigarettes to “less hazardous” other forms of nicotine delivery, particularly e-cigarettes. If e-cigarettes’ main effect for most people is to keep people smoking cigarettes, this policy could end up boomeranging and keeping people smoking cigarettes.
As is evident from the chart above, most of the data are from observational studies of real use, which just two clinical trials, one of which wasn’t even randomized. (There is a third clinical trial, but smoking cessation was not the outcome.) These two or three clinical trials have been the subject of a large number of meta-analyses, including one done by the Cochrane Collaborative. Doing a huge number of meta-analysis of 2-3 studies is just silly.
More important, there is a real question over whether randomized trials are even appropriate for assessing the effects of e-cigarettes on smoking cessation. Randomized controlled trials, in which people are recruited using strict inclusion and exclusion criteria and randomized to receive treatments, then observed going forward are widely accepted as the gold standard for assessing medicines which are administered and monitored by physicians or other health providers as part of a therapeutic effort.
E-cigarettes are not medicines. They are mass-marketed consumer products.
Population studies of use patterns and the effects of product use are more appropriate for assessing the effects of mass marketed consumer products because that reflects what is going on in the real world.
Randomized clinical trials of e-cigarettes as part of a clinically supervised smoking cessation program would make sense (and current FDA rules make doing that impossible in practical terms), but then the results should only be applied to their use under medical supervision (and probably by prescription, given the high abuse potential).

Add new comment